Diabetic Retinopathy
Diabetic retinopathy (DR) is an important cause of visual impairment and blindness in people with Diabetes especially amongst those who fall within the working age group. Thus the morbidity and treatment costs of Diabetic Retinopathy results in significant economic burden to individuals and society as a whole.
Blindness and visual impairment related to Diabetic retinopathy also has significant impact on the quality of life of people with Diabetes.
What is diabetic retinopathy?
Diabetic Retinopathy is a complication associated with Diabetes affecting small blood vessels of the retina. The retina is a light-sensitive layer at the back of the eye that covers about 65 per cent of its interior surface. The optics of the eye creates an image of what is seen on the retina. This functions like the film in a single-lens reflex camera.
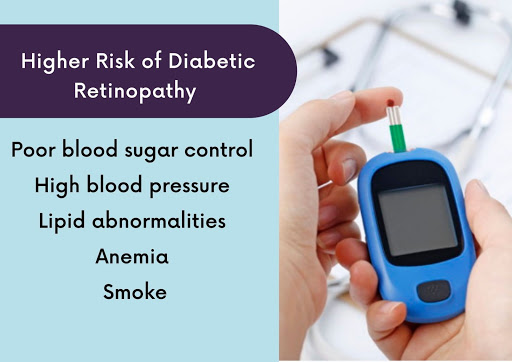
People at a higher risk of developing diabetic retinopathy are those who have:
- had Diabetes for a long duration
- poor blood sugar control
- high blood pressure
- lipid abnormalities
- anaemia
- smoke
How is vision affected by diabetic retinopathy?
In order to understand how vision is affected by diabetic retinopathy, we need to first understand the normal appearance and functioning of the retina. A normal retina is a transparent membrane. When light rays focus on a normal retina, it will result in a clear image.
In diabetic retinopathy, there is increased thickening of the basement membrane resulting in the failure of the pumping mechanism of the blood vessels. This leads to the accumulation of protein deposits in the inner layers of the retina leading to a loss of transparency of the retina which in turn affects vision.
Diabetic retinopathy affects the retina through various stages of severity. Diabetic retinopathy can affect both the macula and the retina. Macula is the central part of the retina and has the highest visual sensitivity required for reading and writing vision. The most common cause of visual loss due to Diabetic Retinopathy occurs when there is fluid accumulation at the macula called diabetic macular oedema (DME).
As diabetic retinopathy progresses from mild to severe forms, the lack of blood supply in the retina results in ischemia (restriction of blood supply to the tissue) and affects the development of new blood vessels as they lack the strength of the original retinal blood vessels. They are smaller and more fragile and can bleed into the gelly (known as vitreous) found in the back cavity of the eyeball. This occurrence is termed as a vitreous haemorrhage.
Initially the patient can experience visual loss in the forms of seeing floaters (cobwebs). Eventually it can lead to the complete blurring of vision. As the severity of diabetic retinopathy progresses, there can be tractional forces acting on the retina resulting in tractional retinal detachment. These advanced stages of diabetic retinopathy can cause irreversible blindness.
Screening for diabetic retinopathy
A trained Ophthalmologist can screen for Diabetic Retinopathy either using Fundus photography or by a dilated fundus examination using indirect ophthalmoscopy.
Recent technological advances in fundus imaging led to a paradigm shift in the screening of Diabetic Retinopathy. These portable indigenous cameras can effectively screen for Diabetic Retinopathy at the primary eye care/ health care settings without the need of an expert. The physician should be the first point of contact for people with Diabetes. 90 percent of Diabetic Retinopathy cases (early stages) only require management (hypertension control and lipid level regulation) under the guidance of a Physician. Only 10 percent of Diabetic retinopathy cases (sight threatening Diabetic Retinopathy) require referral to an Ophthalmologist. Hence visual acuity examination and fundus imaging (portable fundus camera) should be a part of the examination protocol at the physician’s clinic.
Management of diabetic retinopathy
Important modifiable risk factors include glycaemic (blood sugar) control, blood pressure, anaemia, renal parameters, serum lipid level control. Regular physical activity and cessation of smoking does have a positive influence in preventing progression of Diabetic Retinopathy. Regular physical activity in the form of brisk walking, yoga can have a beneficial effect in arresting the progression of Diabetic Retinopathy.
However one with severe form of Diabetic Retinopathy (which has resulted in bleeding in the eye) should be cautious in performing vigorous exercises requiring heavy breathing or lifting heavy weights which can increase pressure on the tiny fragile new blood vessels causing significant vitreous bleeding and resulting in impaired vision.
Medical management of diabetic retinopathy
Laser photo-coagulation is the gold standard therapy in the management of diabetic macular oedema and proliferative (severe) form of Diabetic Retinopathy. Other important options of management include steroid / Anti VEGF injections into the vitreous cavity for the management of diabetic macular oedema and proliferative diabetic retinopathy. These pharmacological advances create a significant impact with regards to visual gain in people with diabetic macular oedema.
Surgical management of diabetic retinopathy
Recent advances in surgical techniques/ visualization systems have changed the scenario of surgical management of Diabetic Retinopathy. The current common indications for surgical management include non-clearing vitreous bleeding, tractional or combined retinal detachment involving macular area. Intravitreal Anti VEGF injections are used as important adjuvants in certain surgical cases of severe forms of Diabetic Retinopathy.
To conclude, good glycaemic control, hypertension and lipid management along with annual diabetic retinopathy screening by fundus examination is essential for preventing blindness and visual impairment caused due to Diabetic Retinopathy.
For more information about Diabetology, safety procedures, and treatment visit our website www.cdi.org.in